New publications
New study reveals key cells that regulate adipose tissue formation
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
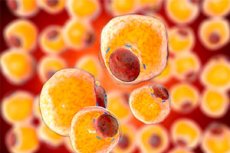
Understanding how adipose tissue forms and functions is critical to combating obesity and related metabolic diseases. However, adipose tissue, or body fat, behaves differently depending on its location in the body.
Take the mesentery, for example: a large, apron-like piece of fatty tissue that hangs from the stomach and covers organs inside the peritoneum, such as the stomach and intestines. Not only does it store fat, but it also plays a role in immune regulation and tissue regeneration.
Mesenteric adipose tissue is associated with an "apple" body shape, which occurs when this fat depot expands significantly, increasing the risk of metabolic disease. This expansion is not due to the formation of new fat cells, a process known as adipogenesis, but mainly through the enlargement of existing cells, a process called hypertrophy. This can lead to chronic inflammation and insulin resistance.
The limited capacity of mesenteric fat to form new fat cells despite a caloric surplus contrasts with subcutaneous fat and remains poorly understood. Now, scientists led by Professor Bart Deplancke from EPFL have identified a cell population in human mesenteric fat that inhibits adipogenesis. The discovery, published in the journal Cell Metabolism, provides new insights into the limited capacity of mesenteric fat to initiate adipogenesis and has significant implications for obesity management.
The researchers used advanced single-cell RNA sequencing to analyze cells from different human fat depots, isolating different cell subpopulations and testing their ability to turn into new fat cells. The study, supported by several medical institutions including CHUV, involved more than thirty human donors to compare the different fat locations in detail.
The approach identified a population of cells present in the mesenteric fat that may be key to explaining its unusual properties. These cells, called mesothelial cells, normally line certain internal cavities of the body as a protective layer.
Among these mesothelial cells, some strangely transitioned closer to mesenchymal cells, which can develop into various cell types, including adipocytes (fat cells). This dynamic transition between cellular states may be a key mechanism by which these cells exert their influence on the adipogenic potential of mesenteric adipose tissue.
The study showed that the mesenchymal-like properties of these cells are associated with an enhanced ability to modulate their microenvironment, providing a regulatory mechanism to limit adipose tissue expansion. By switching between these two states, the cells can thus influence the overall metabolic behavior of the mesenteric fat depot and its ability to accumulate fat without causing metabolic complications.
Importantly, we have also identified at least part of the molecular mechanism by which the new mesenteric cell population influences adipogenesis. Specifically, the cells express high levels of insulin-like growth factor binding protein 2 [IGFBP2], a protein known to inhibit adipogenesis, and secrete this protein into the cell microenvironment. This, in turn, targets specific receptors on adjacent fat stem and progenitor cells, effectively preventing them from developing into mature fat cells."
Radiana Ferrero (EPFL), one of the lead authors of the study "The findings have profound implications for the understanding and potential management of metabolically unhealthy obesity," explains Pernilla Rainer (EPFL), another lead researcher in the study. "Knowing that mesenteric fat has a built-in mechanism to limit fat cell formation could lead to new treatments that modulate this natural process. Furthermore, the study opens up the possibility of targeted therapies that could modulate the behaviour of specific fat depots."
