New publications
New class of oral drug improves embryo implantation and pregnancy outcomes in IVF treatment
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
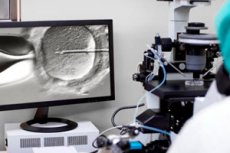
A new study has demonstrated the effectiveness of a first-in-class, oral, non-hormonal drug to increase embryo implantation, pregnancy and live birth rates among infertile women undergoing in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI). The results, presented today at the 40th ESHRE Annual Meeting in Amsterdam, represent a significant step towards the first therapeutic to increase embryo implantation success and live birth rates.
Worldwide, one in six people of reproductive age will experience infertility during their lifetime. More than 3 million IVF cycles are performed each year, and despite advances in IVF technology, embryo implantation failure remains a significant problem.
In response to this unmet need, researchers presented promising results from their Phase 2 OXOART2 clinical trial. This randomized, double-blind, placebo-controlled study, conducted at 28 centers in Europe, evaluated OXO-001, a first-in-class oral drug that acts directly on the endometrium (the inner lining of the uterus) to improve embryo implantation and pregnancy rates.
The OXOLIFE study analyzed 96 women under 40 years of age who underwent a single embryo transfer: 42 received placebo and 54 received a daily dose of OXO-001. Treatment began one menstrual cycle before the embryo transfer cycle and continued until five weeks after the transfer.
Statistically significant improvements were seen in pregnancy biochemical rates – early detection of pregnancy – with rates of 75.9% in the OXO-001 group compared to 52.4% in the placebo group. Clinically significant improvements were also seen in clinical pregnancy rates (fetal heartbeat at 5 weeks post embryo transfer) and ongoing pregnancy rates (10 weeks post embryo transfer), with absolute increases of +14.3 (50.0% for OXO-001 compared to 35.7% for placebo) and +10.6 (46.3% for OXO-001 compared to 35.7% for placebo), respectively.
Most important was the absolute increase of +6.9 in live birth rates (42.6% for OXO-001 versus 35.7% for placebo).
Dr. Agnès Arbat, CEO and Chief Medical Officer of OXOLIFE: “Clinicians and patients know that an absolute increase of more than 5 percentage points in ongoing pregnancy is considered clinically significant. We observed an increase of more than +9, which brings new hope to patients and the scientific community. We look forward to advancing this promising treatment into the next phases of clinical development.”
The incidence of adverse events was similar in both groups. The most common adverse events were headaches, nausea, vomiting, gastrointestinal problems, and dizziness, most of which were mild to moderate. More importantly, there was no difference from placebo in children after six months of follow-up. Overall, OXO-001 was well tolerated, with high compliance rates.
Dr. Ignasi Canals, Chief Scientific Officer of OXOLIFE, adds: “We are excited about the results of this trial, which highlight the potential of OXO-001 to be the first therapeutic option to increase embryo implantation success using a non-hormonal drug with a novel mechanism of action that acts directly on the endometrium.”
Professor Dr Karen Sermon, Chair of ESHRE, explains: "Despite ongoing developments in ovarian stimulation, embryo manipulation and culture, improvements in live birth rates in assisted reproduction have been gradual at best. An increase of almost 7% is very good news for our patients and we hope this will be confirmed in larger patient groups."
An abstract of the study will be published today in the journal Human Reproduction, one of the world's leading journals on reproductive medicine.
