New publications
New chemotherapy drug formula opens doors to advanced cancer treatments
Last reviewed: 23.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Classic paclitaxel formulations - Taxol (in Cremophor EL) and Abraxane (albumin-bound form) - save lives, but are limited: the former causes hypersensitivity due to solvents, the latter poorly penetrates tumors. Researchers from Arizona and colleagues have introduced a new delivery platform: they covalently linked paclitaxel to sphingomyelin, obtaining self-assembling nanovesicles - "paclitaxomes" (paclitaxome) with increased stability, loading and a cleaner safety profile in experiments on mice. Then they "pumped" the vesicles with a pH-sensitive "switch" for deep penetration into the tumor and a mask with CD47 peptide ("don't eat me") to avoid phagocytosis. In models of triple-negative breast cancer and pancreatic cancer, this platform enhanced the effects of standard combinations of paclitaxel with carboplatin or gemcitabine, prevented relapses after removal of the primary tumor, and prolonged survival of mice.
Background of the study
Paclitaxel is a mainstay cytostatic in triple-negative breast cancer (TNBC) and pancreatic cancer (PDAC) regimens, but its efficacy is limited by the delivery form. Classic Taxol on Cremophor EL causes hypersensitivity up to anaphylactoid reactions, and the albumin-bound form of Abraxane eliminates the solvent, but does not solve the problem of insufficient tumor penetration, especially in dense solid tumors. Adding carboplatin to paclitaxel in TNBC improves relapse-free survival, and in PDAC, paclitaxel (in the form of nab-PTX) is combined with gemcitabine, but toxicity and pharmacokinetic limitations limit the potential of combinations. Hence the demand for carriers that will increase the tolerated dose, deliver the drug deeper into the tumor and reduce the "distribution" to healthy tissues.
The key barriers to any nanodelivery are the variability of the EPR effect in humans and the specifics of the tumor microenvironment. What works in mice often “deflates” in the clinic: permeability and retention of particles vary greatly between types and even regions of human tumors. In PDAC, an additional barrier is the pronounced desmoplastic stromal framework, which impairs perfusion and diffusion of drugs. Finally, the extracellular environment of tumors is acidified (usually pH_e ≈ 6.5-6.9) - this interferes with a number of drugs, but opens up the possibility of pH-sensitive “switches” in carriers for targeted activation of capture and release precisely inside the tumor.
In parallel, engineers are solving the problem of evading the mononuclear phagocytic system: macrophages quickly "eat" particles and clear them into the liver/spleen. One approach is to mask the surface with CD47 ("don't eat me") peptides, simulating the "self" signal and prolonging the circulation of particles (with a caveat on immune safety). On the side of the carrier design, sphingolipids are of interest: sphingomyelin, a natural component of membranes, creates stable bilipid layers, and covalent "attachment" of the drug to the lipid increases loading and controllability of release compared to simply "cramming" the molecule into a liposome.
Against this backdrop, a new paper in Nature Cancer proposes just such a “membrane” strategy for paclitaxel: a sphingolipid-derived nanovesicle (paclitaxome) augmented with a pH-switchable module for deep penetration and CD47 masking to evade phagocytosis. The idea is to circumvent the limitations of Taxol/Abraxane, enhance paclitaxel exposure within tumors, and unlock synergy in clinically relevant combinations (with carboplatin in TNBC and with gemcitabine in PDAC) while reducing systemic side effects.
What exactly was invented and why does it work?
The authors started from membrane biophysics. Sphingomyelin, a natural component of cell membranes, provides a convenient "handle" for chemical cross-linking with the paclitaxel molecule - this is how the SM-PTX conjugate is formed, which itself assembles into a liposome-like bilayer. This dramatically increased drug loading and stability compared to attempts to "shove" paclitaxel into conventional liposomes. To solve the problem of surface distribution over the tumor (EPR effect), an ultra-pH-sensitive azepane probe (AZE) was built into the membrane: in the acidic microenvironment of the tumor, it is cationized, turns on adsorption-facilitated transcytosis and pulls the nanovesicle deeper into the tissue. And in order to live longer in the bloodstream and settle less in the liver / spleen, the surface was covered with CD47 peptide - a "self" signal that suppresses macrophage "appetite". For controlled release of the drug in the tumor, sensitive linkers (ether, disulfide, thioketal) were used under local stimuli - esterases, glutathione, active oxygen forms.
Key design elements
- SM-PTX: covalent pro-conjugate of paclitaxel with sphingomyelin → self-assembling "paclitaxel".
- AZE-probe: pH-switched cationization for deep intra-tissue delivery (transcytosis).
- CD47 peptide: "don't-eat-me" mask against the mononuclear phagocytic system, longer in the bloodstream, less in off-target organs.
- Stress-sensitive linkers: PTX release under tumor conditions (esterases/GSH/ROS).
What was shown on animals (and with what numbers)
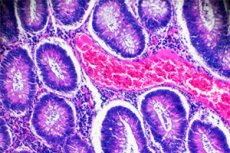
Compared with Taxol and control liposomes, the new formulation significantly increased the maximum tolerated dose of paclitaxel: from 20 mg/kg (Taxol) and 40 mg/kg (the best of the physical liposomes) to 70-100 mg/kg - without noticeable systemic toxicity. In histology, signs of myelosuppression and neurotoxicity (bone marrow, dorsal roots) disappeared at the new MTDs, while standard formulations damaged tissues at their MTDs. In orthotopic models of TNBC (4T1) and pancreatic adenocarcinoma (KPC-Luc), "paclitaxel" as monotherapy inhibited growth more strongly than Taxol/Abraxane, and as co-delivery with carboplatin (for TNBC) or gemcitabine (for prostate cancer) improved intratumoral exposures of both drugs with less distribution among healthy organs. In the postoperative TNBC model, co-nanovesicle with CBPt inhibited recurrence (volume remained ≈35% of preoperative) and significantly prolonged Kaplan-Meier survival.
Best in class comparison
The authors compared their optimized version (CD47p/AZE-paclitaxome) with previously promising nanoforms of paclitaxel - CP-PTX and PGG-PTX. The new platform beat them in pharmacokinetics, accumulation/penetration into the tumor and the final antitumor effect (on the prostate cancer model). Plus, the approach is generalizable: the same modifications of nanovesicles were applied to camptothecin, enhancing its delivery.
Why does oncology need this?
Paclitaxel is a mainstay in TNBC and pancreatic cancer regimens, but its potential is limited by delivery and toxicity. Paclitaxel solves both problems simultaneously: deeper into the tumor, longer in the blood, less in off-target organs, which means room for synergy with partners (CBPt, GEM) without the cost of side effects. At the mechanistic level, co-delivery increased platinum DNA adducts and tubulin stabilization, enhancing apoptosis - exactly what combinations in the clinic are aimed at. If the results are confirmed in large animals and humans, such "membrane" chemistry could become a universal platform for difficult-to-penetrate cytostatics.
Important “buts”: there are still steps to reach patients
This is preclinical work on mice. Questions that need to be answered before the clinic:
- Immune safety of CD47 mask (interference with friend-foe signals), off-target effects.
- Manufacturing and stability: scalability of SM-PTX synthesis and quality control of linkers, shelf life.
- Reproducibility in PDX and large animal models, biodistribution/PK according to GLP, comparison with Abraxane in “fair” dose regimens.
- Combinations are broader than standard (for example, with immunotherapy) and response markers (pH gradients, SIRPα expression, etc.).
What this could mean for patients (carefully)
It is too early to talk about replacing standards: not a single human dose has been administered yet. But for triple-negative breast cancer and pancreatic cancer - diseases with a high risk of early relapse and systemic toxicity from combination chemotherapy - the emergence of a transport platform that simultaneously increases MTD, deepens penetration and reduces side effects looks promising. The next logical step is IND preparation: toxicology, pharmacology, scaling, then phase I with dose escalation and expansion cohorts in combinations.
Source: Wang Z. et al. A sphingolipid-derived paclitaxel nanovesicle enhances the efficacy of combination therapies in triple-negative breast cancer and pancreatic cancer. Nature Cancer (published August 21, 2025). DOI: https://doi.org/10.1038/s43018-025-01029-7
