New publications
The gut microbiome as a key factor in the development of neurodegenerative diseases
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
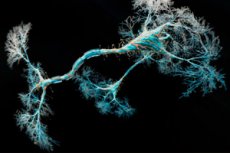
Neurodegenerative diseases (NDDs), for which there are no known cures and whose causes remain unclear, cause irreversible damage to the brain and nervous system. Research into these diseases has typically focused on the brain, but studies in mice over the past few years have suggested that the microbiome also plays a role in the onset and progression of some NDDs.
"These results suggest that the gut microbiome plays an important role in the onset and progression of at least some neurodegenerative diseases," said Chris Ellis, principal investigator of a multi-institutional team of microbiologists from Netellis, the University of Tennessee at Knoxville, and the University of North Carolina at Chapel Hill.
At ASM Microbe, the annual meeting of the American Society for Microbiology, these researchers presented a new link between a metabolite produced by gut microbes and three NDDs in humans. Their analysis suggests that the metabolite DHPS (2,3-dihydroxypropane-1-sulfonate) may help answer key questions about how sulfur metabolic pathways may link the microbiome to these diseases.
DHPS has not previously been detected in humans, and the researchers noted that metabolites produced by gut microbes in NDD patients could offer valuable clues for better understanding, which could lead to improved diagnostic tools or even treatments.
In previous studies, scientists have found that fecal transplants can ease Alzheimer's-like progression in mice, and when fecal transplants from people with the disease are given to mice, the animals experience memory impairment.
The researchers conducted a new study to determine the distinctive bacterial and metabolic profiles of the gut microbiome in people diagnosed with one of three NDDs: amyotrophic lateral sclerosis (ALS), Alzheimer's disease (AD), and Parkinson's disease (PD). To gain early disease data, they collected stool samples from diagnosed patients during their first two specialist visits and compared the results of these samples with samples collected from healthy individuals.
Their analysis identified 19 metabolic biomarkers of neurodegeneration across all three NDD groups; they also found 20 unique markers for ALS, 16 unique markers for AD, and nine unique markers for PD. These common biomarkers included metabolites associated with dyshomeostasis in sulfur metabolic pathways.
In addition, in all three disease groups, they found associations with the bacterial taxa Bilophila and Desulfovibrio, which play a role in the synthesis and degradation of DHPS. The increase in Bilophila levels was consistent with the observation that patients with AD, ALS, and PD had less DHPS in their stool samples compared to healthy subjects.
Bilophila can degrade DHPS to hydrogen sulfide, and hydrogen sulfide accumulation is associated with mitochondrial dysfunction, which is known to contribute to the development of NDD. Hydrogen sulfide is associated with known hallmarks of NDD, including inflammation, oxidative stress, and gut dysbiosis.
The authors suggested that the new study highlights DHPS as a “missing link” in our current understanding of the mechanisms linking NDD to sulfur metabolism, mitochondrial dysfunction, and neuroinflammation.
