New publications
First clinical trial shows safety and efficacy of CAR T therapy for prostate cancer
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Treating prostate cancer with immunotherapy is currently difficult. However, results from the world’s first Phase 1 clinical trial using chimeric antigen receptor (CAR) T-cell therapy developed by researchers at City of Hope®, one of the largest cancer research and treatment organizations in the United States, show that patients with prostate cancer can be safely treated with cellular immunotherapy with promising therapeutic activity, according to a Phase 1 study published today in Nature Medicine.
The study treated 14 patients with metastatic castration-resistant prostate cancer (mCRPC), which has prostate stem cell antigen (PSCA) that has spread beyond the prostate and stops responding to hormonal treatment, with CAR T-cell therapy. More than 34,000 men with this type of prostate cancer die each year in the United States.
Saul Preisman, PhD, assistant professor at City of Hope’s Department of Hematology and Hematopoietic Cell Transplantation, and colleagues developed CAR T cells that target a protein called prostate stem cell antigen (PSCA), which has been found to be highly expressed in prostate cancer patients. The treatment involved taking a patient’s immune cells, called T cells, from the bloodstream and reprogramming them in the lab with CAR to recognize and attack the PSCA protein on the surface of cancer cells. The CAR T cells were then infused back into the patient to kill the cancer cells.
Prostate cancer has been called an immune desert - the tumor nebula is difficult to treat with immunotherapies because there aren't many T cells getting inside the tumor. It takes something really powerful to overcome this. Our study shows that City of Hope's CAR T-cell therapy for prostate cancer may be a step toward achieving this goal."
Tanya Dorff, MD, PhD, is the division director of City of Hope's Genitourinary Diseases Program and a professor in the Department of Medical Oncology and Therapeutic Research.
"The key finding of our study is that PSCA-targeted CAR T cells are safe and effective against mCRPC," Priceman added. "This opens the possibility of further development of this type of cellular immunotherapy for these patients who currently have no other effective treatment options."
The objectives of the trial were to investigate the safety of therapy and dose-limiting toxicity, as well as to obtain preliminary data on the efficacy of treatment in patients.
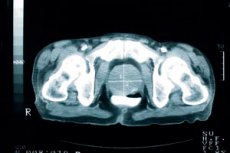
The study’s outcome: Patients received a single infusion of 100 million CAR T cells without prior lymphodepletion chemotherapy, which is routinely used to treat blood disorders to boost the effectiveness of CAR T-cell treatments. Because this was the first-ever clinical trial of CAR T cells, it was important to evaluate the safety of CAR T cells alone in patients. With the same dose of CAR T cells and lymphodepletion, a dose-limiting toxicity complication of cystitis, or bladder irritation, occurred. Dorff explained that PSCA is also present in the bladder, so the CAR T cells likely attacked bladder cells, causing inflammation. The researchers then added a new group to the study with reduced lymphodepletion, which mitigated this toxicity. Four of the 14 patients had a decrease in PSA levels, a serial marker of disease progression in prostate cancer patients, including one patient with a significant decrease. The images showed treatment responses in a subset of treated patients. Five of the 14 patients had mild to moderate cytokine release syndrome, which can be caused by a large, rapid release of cytokines into the blood from immune cells and is a common side effect after treatment with CAR T cells. CRS is a treatable side effect. The CAR T cells did not persist at high levels beyond the 28-day observation period, limiting the effectiveness of the treatment. This represents a common problem in the field of CAR T cells for treating solid tumors, which the researchers plan to address in a follow-up study in City of Hope using a therapy that is now available for enrollment. One patient, who had already undergone several previous therapies, responded favorably to CAR T cell therapy. His PSA levels dropped by 95%, and the cancer in his bones and soft tissue also shrank. He experienced these positive responses for about eight months.
"The patient's results were very encouraging, and we are deeply grateful to him for participating in our study, as well as to the other patients and their families," Dorff said. "We want to continue with this therapy and increase the number of CAR T cells, and also continue to closely monitor any health problems, as we believe this may improve the effectiveness of the treatment."
A phase 1b clinical trial using PSCA CAR T-cell therapy in combination with radiation therapy to enhance anti-tumor activity aims to enroll up to 24 patients.
City of Hope, a recognized leader in CAR T-cell therapy, has treated nearly 1,500 patients since initiating its CAR T therapy program in the late 1990s. The institution continues to have one of the most extensive CAR T-cell therapy clinical trial programs in the world, with nearly 70 CAR T-cell clinical trials currently underway, including 13 different types of solid tumors. The trials utilize City of Hope-developed therapies and products from industry. A recent study published in Nature Medicine introduced City of Hope’s CAR T-cell therapy for brain tumors.
