New publications
AI detects early stage prostate cancer missed by pathologists
Last reviewed: 23.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
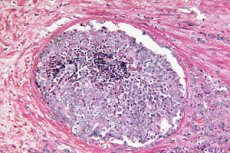
Scientific Reports demonstrates that artificial intelligence can recognize hidden morphological clues of tumor in prostate biopsies that were previously considered benign by a pathologist. A deep learning model trained using the weakly supervised approach predicted which men with elevated PSA would develop clinically significant prostate cancer (ISUP > 1) in the next 30 months and which would remain cancer-free for at least 8 years. This opens the door to early risk stratification immediately after an initial “clean” biopsy and may help decide who really needs repeat invasive procedures and enhanced surveillance.
Background of the study
Primary needle biopsy of the prostate often yields false-negative results: a significant proportion of clinically significant cancer remains “off-screen”, especially with traditional systematic TRUS biopsy. The introduction of MRI guidance has increased the proportion of clinically significant cancer detection and reduced the number of unnecessary repeat procedures, but even with modern strategies, some aggressive tumors remain undetected. The clinical dilemma remains the same: who should be observed after a “clean” biopsy and who should be referred for an early repeat biopsy, so as not to delay diagnosis and not overload patients with invasive interventions.
The biological basis for solving this problem is the TINT (tumor-instructed/indicating normal tissue) phenomenon: a tumor “reconfigures” the surrounding seemingly normal tissues of the organ, leaving in them weak but systematic traces - from stromal remodeling and hypoxia to metabolic shifts. These changes have been described in experimental models and in patients with prostate cancer and correlate with tumor aggressiveness, which makes “normal” tissue a potential source of diagnostic signals, even if there are no obvious cancerous glands in the biopsy core.
Digital pathology and deep learning methods are aimed at extracting such “subtle” field features from standard H&E sections. Unlike classical morphology, which focuses on obvious tumor structures, algorithms can capture distributed patterns in the stroma and epithelium associated with the presence of a tumor in another part of the organ. This opens the way to risk stratification immediately after a negative biopsy: a high glass “score” suggests the advisability of an early repeat biopsy or MRI guidance, a low one supports more gentle observation.
This is the idea behind a new study in Scientific Reports: the authors tested whether AI can predict clinically significant prostate cancer in the next 30 months based on morphological cues from TINT biopsies. The work builds on the line of a previously presented preprint and forms an applied basis for the implementation of “field” digital biomarkers in patient routing after an initial “clean” biopsy.
How it was done: design, data, algorithm
The authors retrospectively collected a cohort of 232 men with elevated PSA and an initial conclusion of "benign" on needle biopsy (after technical control, 213 patients and 587 sections were included in the final analysis; biopsies 1997-2016, Umea, Sweden). Each patient was matched with a "mirror" pair by age, year of diagnosis and PSA level: half were diagnosed with prostate cancer later (≤30 months), the other half remained cancer-free for at least 8 years. H&E slides were digitized (20×), cut into 256×256 pixel tiles and fed to CLAM (Clustering-constrained Attention Multiple-Instance Learning) - a modern weakly supervised scheme, where only the fate of the patient is known, and not the marking of each pixel. Features were extracted by ResNet18 pre-trained on 57 histopathology datasets. The endpoint is binary: low risk (benign/ISUP1) vs. high risk (ISUP2-5).
Prediction accuracy
In an independent test, the model achieved an AUC of 0.81 across slides and an AUC of 0.82 at the patient level. At a threshold that provided an acceptable balance, the sensitivity was 0.92 with a false-positive rate of 0.32 (patient-level). In other words, among people whose initial biopsy “missed,” the AI correctly flagged the vast majority of those who were soon confirmed to have clinically significant cancer, albeit at the cost of some false alarms. For the clinic, this is a signal: “benign” biopsy response ≠ zero risk, and it can be quantitatively stratified by digital glass.
What exactly does AI “notice” in “normal” tissue?
Interpretation via UMAP and attention maps showed that stromal changes are the most informative:
- More collagen in the stroma (matrix compaction, “fibrosis”);
- Fewer smooth muscle cells around the glands;
- Less common are subtle signals in the glandular epithelium, probably below the available downsampling resolution.
This pattern fits into the TINT (tumour-instructed/indicating normal tissue) concept: even the "norm" in an organ where a tumor is hidden is reconfigured under its influence and differs from the "norm" in an organ without a tumor. Cancer is not only a nidus, but also a field, and AI learns to read the field-effect.
How the approach is useful in practice - potential scenarios
- Risk-based re-biopsy: high AI rate on "clean" glass - argument in favor of early re-biopsy or MRI guidance instead of waiting.
- Personalization of monitoring: Low speed counterbalances anxiety after “borderline” MRI and allows moderation of monitoring intensity.
- TINT pattern training: Attention maps and interactive overlays help pathologists see subtle fields around cancer, improving the consistency of reports.
It is important to understand the limitations
It is a single centre in northern Sweden (predominantly Caucasian population), the design is retrospective, the baseline biopsies were performed without MRI guidance (systematic TRUS biopsies), and the markers are future outcomes rather than "occult tumor on the same slide". There is no external validation at independent centres/scanners yet, nor is there a prospective trial of the effect of the algorithm on clinical decisions and outcomes. The false positive rate remains significant - the model does not replace the physician but adds a probabilistic layer for shared decision-making.
What's Next: Implementation Roadmap
- Multicenter external validation (different scanners, protocols, ethnic groups).
- Prospective decision studies: does AI score change patient trajectory (time to diagnosis, number of unnecessary repeat biopsies, over/under-diagnosis).
- Integration with MRI and clinic: combined models (PSA, MRI PIRADS, clinical factors + TINT score according to H&E).
- Technical steps: standardization of digitalization, control of data drift, explainability (attention overlays for routine).
Source: Chelebian E., Avenel C., Järemo H., Andersson P., Bergh A., Wählby C., et al. Discovery of tumor indicating morphological changes in benign prostate biopsies through AI. Scientific Reports (Nature Portfolio), published 21 August 2025. DOI: https://doi.org/10.1038/s41598-025-15105-6
