Medical expert of the article
New publications
Examination of the respiratory system
Last reviewed: 23.11.2021

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Despite the great successes in the development of special methods for studying the state of respiratory organs, many of the methods of physical examination still described by R. Laennec are still of paramount importance. However, now we try to identify only those symptoms that really have an important diagnostic value, while realizing that in some lung diseases (for example, bronchogenic cancer or tuberculosis), the onset of these symptoms often indicates a sufficiently pronounced stage of the disease, and for early diagnosis it is necessary to use more subtle methods.
Another difference of the modern stage of the respiratory system research is a much greater attention to the physiology of breathing, the relationship between clinical signs and impairments of the function of external respiration, to functional, and not just anatomical changes.
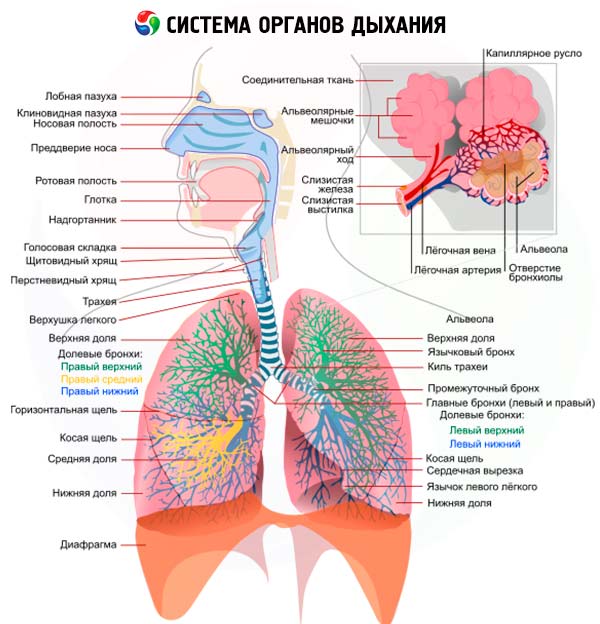
The modern stage of understanding the pathological processes that arise in the respiratory organs is impossible without the knowledge of those protective mechanisms that prevent the penetration of microorganisms, dust particles, toxic substances, pollen of plants, etc. In addition to anatomical barriers (larynx, epiglottis, numerous divisions and narrowing of the bronchial tree ), a rich vascularization of the mucous membrane of the respiratory tract, a cough reflex, a very important role in the protection of respiratory organs is played by mucociliary transport, carried out by ciliated ep teliem bronchi and formation tracheobronchial secretions containing biologically active substances (lysozyme, lactoferrin, a1-antitrypsin) and synthesized by plasma cells of all classes of immunoglobulins, but primarily IgA. At the level of terminal bronchi, alveolar courses and alveoli, protective function is performed mainly by alveolar macrophages and neutrophilic granulocytes with their pronounced chemotaxis and phagocytosis, as well as lymphocytes that release lymphokines that activate macrophages. Broncho-associated lymphoid tissue (BALT), like the responses of humoral (immunoglobulin classes A and G) immunity, are of particular importance in the protective mechanisms of the respiratory system. An important place in protecting the lungs is their full ventilation.
All these mechanisms of respiratory protection can now and should be studied in each individual patient, which allows us to provide more details of the features of the developing disease, and therefore, choose a more rational treatment.
In the study of the respiratory system (which, as in all other cases, begins with questioning, and then the examination, palpation, percussion and auscultation are performed ), the main question to be answered is the determination of the primary localization of the process: the respiratory tract, lung parenchyma or pleura. Often, several parts of the respiratory system are involved: for example, with inflammation of the lobe of the lung (lobar, or croup, pneumonia ), there is almost always an inflammation of the pleural sheets ( pleurisy ), with focal pneumonia, the process usually begins with bronchitis ( bronchitis ), and then develop peribronhialnoe inflammation. This makes the clinical picture of a number of pulmonary diseases diverse and makes it necessary to assess the detected signs from different perspectives.
Anamnesis of the disease in diseases of the respiratory system
Continuing interrogation allows to reveal the features of the development of pulmonary pathology - anamnesis of the disease. The general principle of "not to spare time to get acquainted with an anamnesis" should be fully used in the study of diseases of the respiratory system. The time sequence of the appearance of these or other signs of the disease, the peculiarities of its initial period, relapses, their frequency and the presence of provoking factors, the nature and effectiveness of the treatment, the appearance of complications are specified.
Thus, in acute pulmonary diseases, general symptoms such as malaise, chills, fever can be detected several days before the pulmonary signs (viral pneumonia) or almost simultaneously with them ( pneumococcal pneumonia ), and acute acute dyspnea is a very important sign of bronchial asthma, acute respiratory failure, as well as pneumothorax. It is necessary to evaluate the results obtained with the help of special research methods (sputum analysis, blood tests, radiography, etc.). Of particular importance are indications of the presence of allergic reactions (urticaria, vasomotor rhinitis, Quincke's edema, bronchospasm) in response to the effects of factors such as food, odors, medicines (primarily antibiotics, vitamins); Recently, close attention has been paid to the possibility of worsening of the course of bronchial asthma with the use of aspirin and other non-steroidal anti-inflammatory drugs ("aspirin asthma").
An important stage of the questioning is an attempt to establish the etiology of the disease (infectious, professional, medicinal).
A number of serious lung diseases are associated with more or less prolonged contact with various industrial factors, such as dust containing silica, asbestos, talc, iron, aluminum, etc. In addition to the well-known professional pulmonary diseases of the lungs ( pneumoconiosis ) it is now increasingly detected communication such pulmonary diseases as exogenous allergic alveolitis, numerous environmental factors, such as rotting hay, grain raw et al. ( "light farm and "easy cheesemaker," "easy fanciers", etc.). It is not uncommon for diffuse pulmonary changes to occur in patients receiving medicines such as cytostatics, nitrofurans, cordarone and its analogs in various non-pulmonary diseases, as well as long-term radiation therapy.
All the revealed features of the disease course should be eventually presented in the form of an appropriate graphic image, an example of which is the observation of a patient with croupous pneumonia.
Finally, important information can be obtained when studying a family history (family propensity with bronchopulmonary diseases, for example bronchial asthma, tuberculosis or the presence of a1-antitrypsin deficiency, cystic fibrosis ), as well as bad habits: smoking is a recognized risk factor for lung cancer, alcohol abuse contributes to unfavorable course pneumonia (suppuration, abscessing).
Smoking (especially smoking cigarettes) takes a special place in the history of the development of pulmonary disease in each individual patient, as it causes or worsens this disease. Therefore, it is important for the doctor to know (record) the number of cigarettes smoked per day, and the time during which the patient smokes (the so-called "cigarette pack" years). It is in malignant smokers that first of all there are chronic bronchitis and emphysema - severe variants of chronic obstructive pulmonary disease; with smoking directly linked to bronchogenic cancer - one of the most common malignant tumors in men and increasingly appearing in women.
 [1], [2], [3], [4], [5], [6], [7]
[1], [2], [3], [4], [5], [6], [7]
Upper respiratory tract examination
A direct examination of the respiratory system often begins with a survey of the chest. More correct is still to consider a preliminary study of the state of the upper respiratory tract, which is due to the important role that various pathological changes in the upper respiratory tract can play in the development of lung diseases. It goes without saying that a detailed examination of the upper respiratory tract is the responsibility of the otolaryngologist. However, a doctor of any specialty (and above all a therapist) should know the main symptoms of the most common diseases of the nose, pharynx, larynx, and have good knowledge of the simplest methods of examining the upper respiratory tract.
First of all, specify how free the patient can breathe through the nose . To better assess nasal breathing, the patient is offered to close alternately nasal passages, squeezing successively the left and right wings of the nose to the nasal septum. Difficulty of nasal breathing is a frequent complaint of patients and occurs, for example, in the curvature of the nasal septum, acute and chronic rhinitis, sinusitis.
Clarify the presence of the patient's feeling of dryness in the nose, which may appear in the initial stage of acute rhinitis or be noted constantly in patients with chronic atrophic rhinitis. Often there is a complaint of patients for the appearance of discharge from the nose. In such cases, their number is determined (abundant discharge in acute rhinitis, scanty, with crust formation - with atrophic rhinitis), character (serous or mucous discharge - with acute catarrhal rhinitis, watery - with vasomotor rhinitis, thick and purulent - with maxillary sinusitis, - with influenza, etc.), and also note whether the number of left and right nasal passages is equal.
The complaint of patients for the appearance of nasal bleeding, which can be associated with local causes (trauma, tumor, ulcerous nasal mucosa), or are due to some common diseases (for example, hypertension, hemorrhagic diathesis, leukemia, avitaminosis, etc.) deserve much attention. .). In the presence of nasal bleeding, find out how often they occur in the patient (episodically or regularly), whether they are meager or too plentiful. Lean nosebleeds usually stop on their own. Abnormal nasal bleeding (over 200 ml per day) can be accompanied by general symptoms characteristic of all profuse bleedings (general weakness, falling blood pressure, tachycardia), and require emergency measures to stop it (tamponade of the nasal cavity). It should be borne in mind that it is not always possible to correctly establish the volume of nasal bleeding, since the blood flowing down the back wall of the nasopharynx is often swallowed by the patients.
Sometimes patients also complain of a worsening of smell ( hyposmia ) or its complete absence. Odor disorders can be associated with both difficulty in nasal breathing and with damage to the olfactory nerve.
With inflammation of the paranasal sinuses (frontal, maxillary, etc.), pain can occur in the region of the root of the nose, forehead, zygomatic bones, sometimes radiating to the temporal region.
A thorough examination of the nasal cavity is performed by the otorhinolaryngologist with the help of a rhinoscope, which involves the use of special nasal mirrors. However, the anterior section of the nasal cavity can be viewed well enough without resorting to special methods. For this, the patient slightly tilts his head, four fingers (II-V) of the right hand are placed on the forehead of the patient, and the thumb of the same hand is slightly pressed (from the bottom up) to the tip of the nose. Pay attention also to the presence of soreness with palpation and effleurage in the area of the root of the nose, its back, the projection of the frontal and maxillary sinuses of the sinuses. Soreness, as well as swelling of soft tissues and hyperemia of the skin in these areas can occur with damage to the bones of the nose, inflammatory diseases of the paranasal sinuses.
A full study of the larynx is possible only with the use of laryngoscopy, which is performed by a specialist-otolaryngologist. In those cases when the examination of the patient is conducted by a doctor of another specialty, analyze the patient's complaints indicating a possible larynx disease (for example, pain during conversation and swallowing, characteristic barking or, conversely, silent coughing), reveal changes in voice ( hoarseness, aphonia), note respiratory disturbances (loud, stressed, with difficulty breathing), appearing, for example, with stenosis of the larynx.
When examining the larynx, assess possible changes in shape (for example, with trauma); when you feel the area of the larynx determine the presence of swelling or soreness (with traumatic injuries, chondroperichondritis, etc.).
Additional methods of examination of the respiratory system
To clarify the diagnosis, the degree of activity of the pulmonary process (exacerbation, remission), the functional state of the respiratory system, additional methods of clinical examination, such as blood testing (including immunological indices), urine, but especially sputum analysis, bronchoalveolar lavage fluid, pleural fluid, as well as X-ray methods, which in recent years have been supplemented with tomographic and computer tomography studies, radiocontrast (bronchography, angiopulmonography), radionuclide and endoscopic methods (bronchoscopy, thoracoscopy, mediastinoscopy), puncture biopsy of the lungs, mediastinal lymph nodes, special cytological studies. Particular attention is paid to the study of the function of external respiration.
The necessity to use additional methods of investigation is also connected with the fact that in a number of cases, the general examination shows no changes, especially in the early stage of the disease, which do not manifest clinically (for example, bronchogenic carcinoma, a small tuberculous infiltrate). In these cases, the diagnosis depends on the ability to apply additional methods.
 [8], [9], [10], [11], [12], [13]
[8], [9], [10], [11], [12], [13]
Sputum examination
A macroscopic study of sputum was discussed earlier. At a microscopic examination of sputum (stained smears), the prevalence of neutrophils can be detected, which is associated with bacterial infection (pneumonia, bronchiectatic disease, etc.), which in some patients is confirmed by the subsequent detection of microbial growth during sputum culture, or eosinophils, which is considered characteristic of the bronchial asthma and other allergic lung diseases. When bronchial asthma in sputum, you can identify the Kurshman spirals (slime-containing casts of spastic bronchial constriction) and the Charcot-Leiden crystals (presumably the remains of eosinophils). The presence of erythrocytes in the smear testifies to the admixture of blood as a sign of bronchial or pulmonary hemorrhage. Alveolar macrophages can be detected, which indicates that the material is obtained from the deep sections of the respiratory tract. If they contain derivatives of hemoglobin (siderophages, cells of heart defects), one can think of the presence of blood stagnation in a small circle of blood circulation (decompensated mitral heart disease, other causes of heart failure). With general sputum microscopy, elastic fibers can be identified - a sign of destruction of lung tissue (abscess and gangrene of the lungs, tuberculosis), as well as drusen of fungi. The most important method of studying sputum is the identification of bacteria in smears stained by Gram, which provides valuable information about the cause of the inflammatory process, primarily pneumonia, and allows for more targeted initiation of etiologic treatment.
Investigation of the lavage fluid
In recent years, a microscopic study of the fluid obtained from flushing (from English lavage) by an isotonic solution of the walls of subsegmental bronchi, a broncho-alveolar lavage fluid (BALF), is being widely used, which is aspirated by the same bronchic fibroscope that was used to instill the solution. The normal cellular composition of BALWH in non-smokers is 100-300 ml of the fluid mainly by alveolar macrophages (up to 90%), stabilized leukocytes (1-2%), lymphocytes (7-12%), and bronchial epithelial cells (1-5%) . Due to changes in the cellular composition of BALF, activity of alveolar macrophages, a number of other immunological and biochemical indicators, important diagnostic findings are made. For example, with such a commonly encountered diffuse lesion of the lungs as sarcoidosis, BALM predominates lymphocytes over neutrophils; detection of fungi, pneumocyst allows to diagnose rare variants of bronchopulmonary infection.
Pleural puncture
A definitive diagnostic value is the study of fluid obtained with the help of pleural puncture. Determine its appearance (light, transparent, cloudy, purulent, bloody, chyle), odor, relative density of protein content. In the presence of exudate (in contrast to the transudate), the relative density and protein content of the resulting liquid are high, respectively, greater than 1.015 and 2.5%; Currently, instead of the Rivolta sample, the ratio of the protein content in the pleural fluid to the plasma protein content is used (in the presence of exudate it is greater than 0.5).
X-ray methods of research
Particularly important in the diagnosis of respiratory diseases are x-ray methods that confirm the diagnostic assumptions that arise at the previous stages of the survey, are reliable in dynamic observation, in some cases help clarify the etiology of the disease even before the results of bacteriological and cytological studies. The significance of radiological methods in determining the localization of pulmonary changes and understanding the essence of the process is unconditional. For example, bronchopneumonia and fungal lesions can be determined in any part of the lungs, lobar and segmental changes are primarily characterized by pneumonia, lung infarction, endobronchial tumor growth.
Currently, fluoroscopy is used much less often, since it has a higher radiation load, the interpretation of changes is subjective in many respects, comparative dynamic observation is difficult, although the use of a television screen and video recording of an image avoid some negative aspects. The advantage of this method is the possibility of studying the lungs in the process of breathing, in particular the movements of the diaphragm, the state of the sinuses, the position of the esophagus.
Radiographic ( fluorographic ) research is the most objective, widespread and essentially the main method of additional research, which allows obtaining accurate data and evaluating them in dynamics. The use of oblique, lateral positions, the position of lordosis (to identify apical localizations), etc. Helps to clarify the diagnosis. At the same time, features of pulmonary parenchyma, vascular and interstitial structure (pulmonary pattern) are analyzed, the roots of the lungs and a number of other parts of the respiratory system are evaluated. More detailed changes are specified in tomography and computed tomography. These methods allow to reveal the pathology of bronchi, trachea (in particular, its bifurcation), seals located at different depths. Especially informative in this respect is computed tomography, which, thanks to the use of a computer that simultaneously processes data of hundreds of translucencies of a certain layer of tissue in a short time, provides information on very small and difficult to access for conventional radiology studies.
X-ray methods include contrast angiopulmonography with the introduction of iodine-containing substances (urotranscript, verographin), through which the features of the vessels of the small circle of blood circulation, as well as arteries of the bronchial tree, are revealed.
The data obtained using radionuclide methods: the introduction of radioactive isotopes and the subsequent evaluation of their distribution in the organs of the thorax using special apparatus (scanners, gamma camera, etc.) have definite diagnostic significance. Pulmonary practice usually uses radioactive isotopes of technetium ( 99 Tc), in particular technetium-labeled albumin, gallium ( 67 Ga), xenon ( 133 Xe), indium ( 133 In), phosphorus ( 32 P). Radionuclide methods allow evaluating perfusion properties (technetium), regional ventilation (xenon), proliferative cellular activity of interstitium, lymph nodes (gallium). For example, this study reliably detects perfusion disorders in pulmonary embolism, the accumulation of the gallium isotope in the lymph nodes of the mediastinum with active sarcoidosis.
Endoscopic methods of research
A special place in the examination of a patient with lung disease belongs to endoscopic methods, among which bronchoscopy is of primary importance . Using the modern bronchic fibroscope, it is possible to visually evaluate the features of the airways from the glottis to the subsegmental bronchial tubes, the function of the mucociliary escalator, take the contents of the respiratory tubes at different levels for cytological and bacteriological studies, perform bronchoalveolar lavage, then study the flush, make a puncture biopsy of the bronchial mucosa, as well as transbronchial biopsy of adjacent tissues (lymph node, lung). Bronchoscope is used for therapeutic purposes, sometimes for flushing bronchial tubes and for local administration of antibacterial agents for bronchiectasis (bronchial cleansing), but especially for diluting and sucking off mucus from the lumen of blocked bronchi with an uncombined bronchial asthma attack, especially if there is a picture of "mute lung" removal of a foreign body.
 [14], [15], [16], [17], [18], [19], [20], [21]
[14], [15], [16], [17], [18], [19], [20], [21]
Indications for bronchoscopy
|
Indications |
Notes |
|
Hemoplegia. |
To establish the source (preferably in a period close to the end of bleeding) and to stop bleeding. |
|
Chronic cough for no apparent reason. |
There may be an endobronchial tumor that is not visible on the roentgenogram. |
|
Slowed-down resolution of pneumonia. |
To exclude local bronchial obstruction. |
|
Atelectasis. |
To establish the cause. |
|
Lung cancer. |
For biopsy, evaluation of operability. |
|
Abscess of the lung. |
To exclude obstruction of the bronchus, obtain material for bacteriological examination and to improve drainage. |
|
Foreign body. |
For removing. |
Bronchoscopy is mandatory in patients with hemoptysis (especially repeated) or pulmonary hemorrhage, it allows you to establish the source (trachea, bronchi, parenchyma) and the cause (bronchiectasis, swelling, tuberculosis) of bleeding.
Among other endoscopic methods, although rarely, thoracoscopy (examination of pleura sheets) and mediastinoscopy (examination of the anterior mediastinum) are used, one of whose main goals is biopsy of the corresponding sites.
Ultrasound examination (ultrasound)
In pulmonology, ultrasound is not yet very informative, it can be used to identify small areas of exudate and perform pleural puncture.
Intradermal tests
In the diagnosis of certain pulmonary diseases, intradermal tests are used that help determine the presence of atopy (for example, allergic rhinitis, certain variants of bronchial asthma), the cause of pulmonary eosinophilia; The tuberculin test (especially in children's and adolescent practice), the Kveim test (in the diagnosis of sarcoidosis) are of diagnostic importance .
Examination of respiratory function
Assessment of the functional state of the respiratory system is the most important stage of the examination of the patient. Lung functions are very diverse: gas exchange, regulation of the acid-base state, heat exchange, water metabolism, synthesis of biologically active products, but one of the main functions of the respiratory system is the function of gas exchange, which includes the entry of air into the alveoli (ventilation), gas exchange in the alveoli (diffusion ), oxygen transport by the blood of the pulmonary capillaries (perfusion). Therefore, a special place in the study of respiratory organs is the study of the function of the apparatus of external respiration. The normal functioning of this system ensures gas exchange between the external and internal environment, which means that it determines the usefulness of tissue respiration, which is why it is important to understand the role of all components of the external respiration mechanism. The clinician needs to establish the functional capacity of this system, i.e., to detect the degree of respiratory failure.
The most important method for determining the function of external respiration, primarily the ventilation function, is spirography. Basic spirographic indicators (pulmonary volumes) are divided into static and dynamic. The first group includes the volumetric parameters. First of all, this is the vital capacity of the lungs (JEL), i.e., the volume of air at the maximum expiration produced after the maximum inspiration. Of the dynamic indicators, the forced vital capacity of the lungs (FVC) - the air volume with the most intense and rapid expiration, which is 80-85% YEL for the first second of exhalation (Tiffno test) is of special importance. FVC affects the state of bronchial patency: the smaller the clearance of the bronchi, the more difficult the exhalation, the smaller the volume of forced expiration.
Another dynamic indicator - the volumetric rate of forced inspiration and expiration (normally 5-7 l / s) and with quiet breathing (at a norm of 300-500 ml / s) - is determined by a special device with a pneumotachometer and reflects the state of bronchial patency: a decrease in the expiratory flow rate is a sign bronchial obstruction.
Speed indicators of breathing are represented graphically by plotting the "flow-volume" curves, at which each of the points corresponds to a certain percentage of the FVC: the ordinate delineates the air flow rate (in liters per 1 s), abscissa - the forced expiratory volume (in percent or liters) and determine the peak and instantaneous space velocities (MOS) of the flow at the time of forced exhalation. With bronchial obstruction, the curve is shifted to the left and has a flat end part, with the restriction of the lungs it is shifted to the right and does not differ in shape from the norm.
The diffusion capacity of the lungs can be determined with the help of carbon monoxide (CO) flowing through the membrane (like O2): when breathing in CO, the diffusion rate is calculated, which decreases (sometimes significantly) with severe lesions of the alveolar membrane and lung interstitium.
When assessing respiratory function, the determination of the partial pressure of oxygen and carbon dioxide, as well as the pH of arterial blood, is of great clinical importance.
Assessment of the state of the capillary bed (perfusion or transport of oxygen by blood) is carried out by inhaling pure oxygen: insufficient after inhalation increase of PO 2 in the arterial blood indicates a poor perfusion ability of the lungs.

