Medical expert of the article
New publications
Esophagus
Last reviewed: 19.11.2021

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
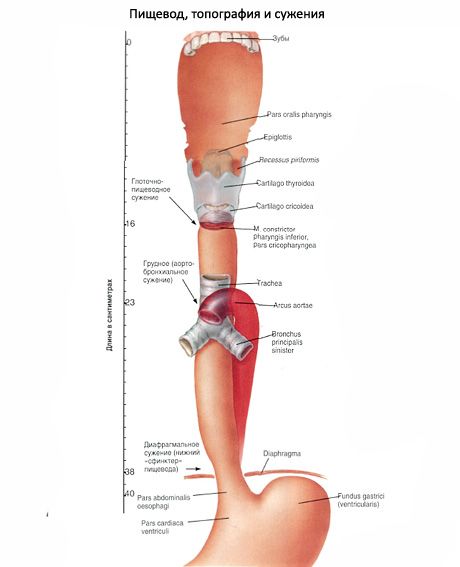
Esophagus (oesophagus) is a hollow tubular organ that serves to carry food masses from the pharynx to the stomach. The length of the esophagus in an adult is 25-27 cm. The esophagus is somewhat flattened in anteroposterior direction in its upper part, and in the lower part (below the level of the jugular notch of the sternum) resembles a flattened cylinder. The esophagus begins at the level of the pharyngeal-esophageal transition at the level of the V-VII cervical vertebrae and flows into the stomach at the level of the IX-XII thoracic vertebrae. The lower border of the esophagus in women is usually located on 1-2 vertebrae higher than in men.

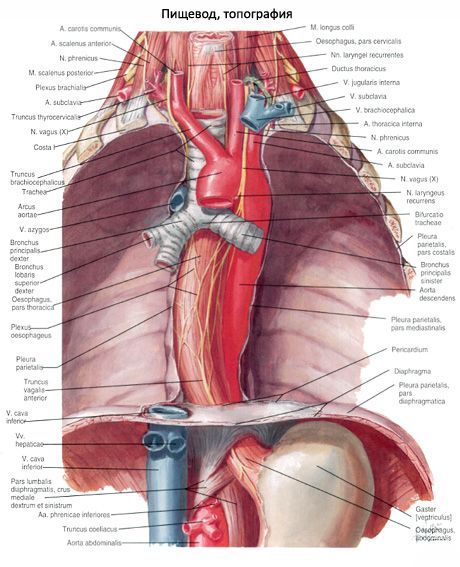
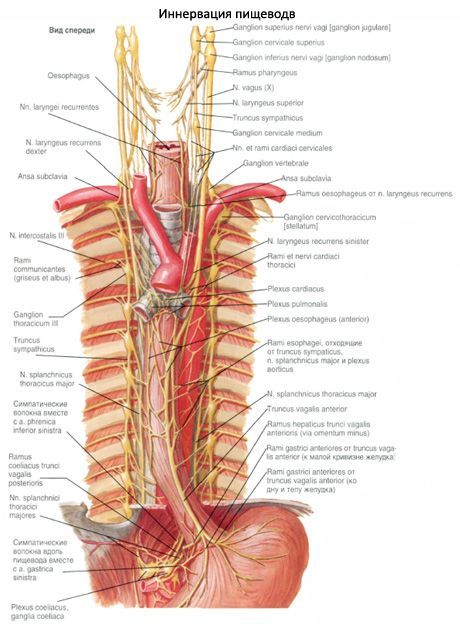
The neck part of the esophagus (pars cervicalis) has a length of 5-7 cm. It is surrounded by a loose connective tissue, passing down into the fiber of the posterior mediastinum. In front of the neck part of the esophagus is the membranous wall of the trachea, from which the esophagus is closely connected by a loose fibrous connective tissue. The left recurrent laryngeal nerve usually passes from the anterior surface of the neck part of the esophagus. The right recurrent guttural nerve usually extends along the right side surface of the esophagus, behind the trachea. Behind the esophagus is attached to the spine and the long neck muscles, covered with a vertebral plate of the cervical fascia. On the side of the neck part of the esophagus, on each side there is a neurovascular bundle (common carotid artery, internal jugular vein, vagus nerve).
Thoracic part of esophagus
(pars thoracica) has a length of 16-18 cm. Anteriorly from the esophagus in the thoracic cavity are successively located the membranous wall of the trachea, below - the arch of the aorta, the beginning of the left main bronchus. Between the posterior wall of the trachea, the left main bronchus on one side and the esophagus - on the other are muscle and connective tissue bundles of unstable bronchopiscus muscles and ligaments. Below the esophagus passes behind the pericardium, that part of it that corresponds to the level of the left atrium.
Behind the thoracic part of the esophagus is the spine (up to level III-IV of the thoracic vertebrae). Below, behind the esophagus and just to the right of it, is the thoracic lymphatic duct, even lower is the semi- unpaired vein.
The relationship between the esophagus and the aorta is complex. The aorta first contacts the left surface of the esophagus, passes between it and the spine, and in the lower parts the thoracic part of the esophagus lies in front of the aorta.
From the sides to the thoracic part of the esophagus below are vagus nerves. The left nerve passes on the left side closer to the front surface, and the right one - closer to the back surface of the esophagus. At the level II-III of the thoracic vertebra, the right surface of the esophagus is often covered by the right mediastinal pleura.
From the right surface of the lower third of the thoracic part of the esophagus to the right mediastinal pleura is the so-called pleuropischevnaya muscle.
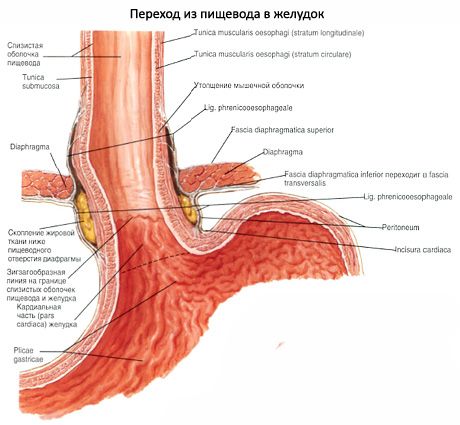
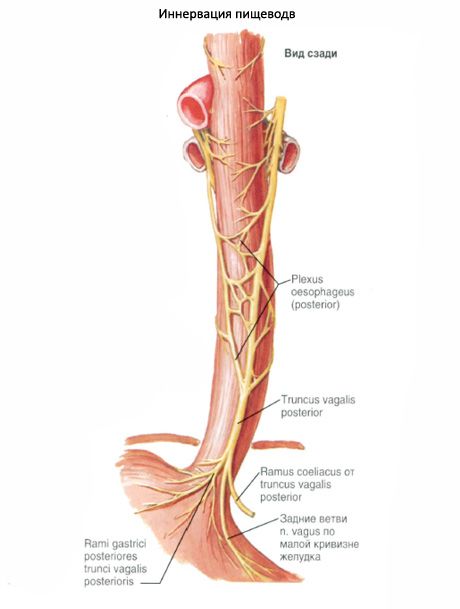
The abdominal part of the esophagus (pars abdominalis), having a length of 1.5-4.0 cm, from the esophagus of the diaphragm to the area of transition into the stomach goes obliquely down and to the left. Esophagus in the abdominal cavity comes into contact with the left leg of the lumbar part of the diaphragm, in front - with the tail of the liver. The left vagus nerve is located on the anterior wall of the esophagus, the right one on the back. In 80% of cases the esophagus in the abdominal cavity is covered with the peritoneum from all sides, in 20% of cases its posterior wall is devoid of peritoneal cover.
Esophagus does not have a strictly straight path, it forms small bends. The esophagus is located on the middle line to the level of the sixth cervical vertebra, then makes a weak bend to the left in the frontal plane. At the level II-III of the thoracic vertebra, the esophagus is shifted to the right to the midline. Anteroposterior bend of the esophagus is located between the level of the sixth cervical and 2nd thoracic vertebrae (corresponds to the bend of the spine). Below the level II of the thoracic vertebra, the esophagus again forms a bulge in front (due to proximity to the aorta). When passing through the diaphragm, the esophagus deviates anteriorly.
The esophagus has narrowing, which is located in the area of the pharyngeal esophagus, behind the aorta (level IV of the thoracic vertebra) and in the region of the esophageal opening of the diaphragm. Sometimes there is constriction behind the left main bronchus.
The wall of the esophagus consists of four layers: the mucosa, the submucosa, the muscular and adventitious membranes (Figure 225). The wall thickness is 3.5-5.6 mm.
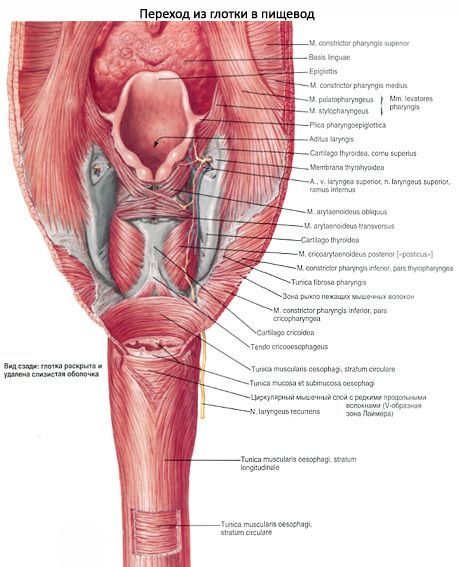
The mucosa (tunica mucosa) of the esophageal wall is lined with multilayer, flat, non-coring epithelium (25-35 layers of epithelial cells). At the level of the upper third of the esophagus, the thickness of the epithelium is somewhat less than in the remaining parts of the organ. The basal membrane (0.9-1.1 μm thick) is fenestrated. The propria of the mucous membrane is well defined, forming numerous papillae that protrude deep into the integument epithelium. In the upper and especially in the lower parts of the esophagus there are cardiac glands similar to the stomach glands of the same name (contain mucous and in an insignificant number of parietal and endocrine cells). The thickness of the own plate in the zones of the location of the cardial glands significantly increases. The muscular plate of the mucous membrane thickens in the direction from the pharynx to the stomach.
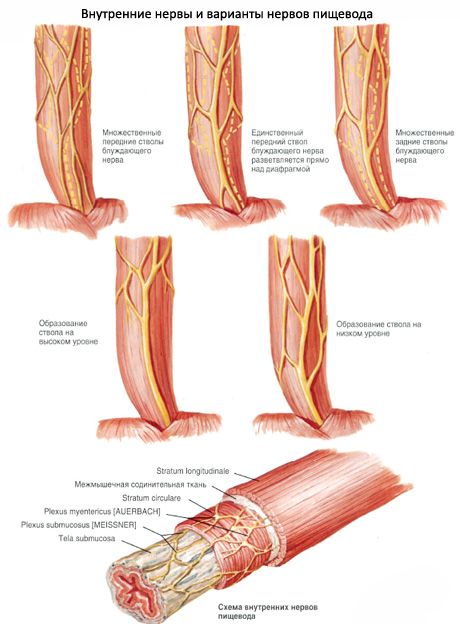
The submucosa of the esophagus (tela submucosa) is well developed; it promotes the formation of 4-7 pronounced longitudinal folds of the mucosa. In the thickness of the submucosa base, along with vessels, nerves, cells of various nature (lymphoid, etc.), there are 300-500 multicellular alveolar-tubular glandular mucosal glandular types. These glands contain separate endocrine cells.
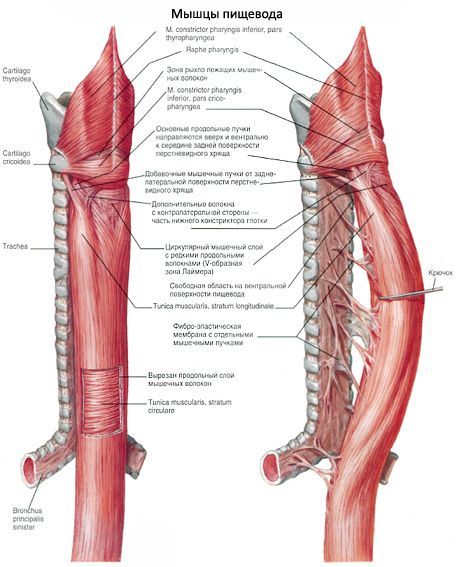
The muscular membrane of the esophagus (tunica muscularis) is represented in the upper third by transversely striated muscle fibers. In the middle part of the esophagus they are gradually replaced by smooth myocytes. In the lower part of the esophagus, the muscular membrane consists entirely of bundles of smooth myoins. Muscle fibers and myocytes are arranged in two layers: the inner layer is annular, the outer layer is longitudinal. In the neck part of the pedicle, the annular layer is 2 times thicker than the longitudinal layer. In the thoracic part, both layers are equal in thickness, in the abdominal - the longitudinal layer predominates in thickness. The muscular membrane determines both the peristalsis of the esophagus and the constant tonus of its walls.
Adventitia (adventitia) covers the esophagus from the outside. The most favorable is the adventitia over the diaphragm. At the level of the diaphragm, the adventitia is substantially compacted by fibrous fibers associated with the fascial fibers of the diaphragm. The abdominal part of the esophagus is completely or partially covered by the peritoneum.
 [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14]
[1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14]

